I was so privileged to be interviewed by Samantha Stephenson for her Brave New Us podcast! This episode is about genetic illness and genetic manipulation: Should we do it? Why or why not? I had a great time talking to Samantha and I hope you enjoy our conversation! You can listen here.
CF
How to be your own health care advocate
CF, essays, health, how to, transplantCommentToday I’m going to share some hard won wisdom with you!
A friend of mine who also has CF said that we’re the “marines of health care.” And that’s true. We’ve had decades of experience working closely with doctors, hospitals, and medication regimens. And what we think of as obvious is not so obvious to the rest of humanity.
So I’m going to share some tips with you today to help you have better health!
I’m going to start with what is probably the most important tip:
Know your baseline.
What I mean by that is know yourself. How do you normally feel? What’s your general energy level? How much sleep do you normally need—and get—and what do you feel best with? (For me, it’s about nine hours.) How does caffeine affect you? (Or doesn’t it?)
All these things are your baseline—how you normally feel when you’re healthy and everything is chugging along just fine. This even includes stuff like how many times you normally go to the bathroom. (I’m not kidding. For a diabetic, this is important to know—and same with CF.)
You might not have thought about this before, but when you feel “off”, it’s because you’re unconsciously comparing your state to how you normally feel—aka, your baseline.
For example, my right hip tends to bother me on and off. It’s not a big deal, I’m aware of it, it’s been checked out. But if it suddenly became really painful, that would be an anomaly.
I knew that my blood glucose was really high, without even testing it, when I was dropping weight really easily and going to the bathroom more often, and carrying water around with me. Those are all not normal feelings for me.
Knowing how you feel—both physically and emotionally and mentally-is key to judging if something is wrong with you.
I knew that the type of insulin I was on over the summer was wrong for me—on a lot of levels—because I became a really awful person! I was snappy and lost my temper at everything and just hated everything, and this is not me!
So you have to know how you feel normally, so you know how you feel when you’re sick, or when something is off.
All drugs have side effects
The questions are: will you get side effects, and if you do, how bad are they?
People are generally shocked to hear that meds can cause problems. Yes, they can. Heck, water can cause problems if you drink too much of it. If you take too much Tylenol, your kidneys are not gonna be happy with you!
Every medication has side effects. Not every person will experience any, or all, of them.
But a side effect alone is not enough to not take the med.
For example: I used to take cipro for infections. People were always shocked. “Don’t you know that class of meds can cause tendon issues?!” they would cry.
Well, yes, I did (do) know that. But the thing is, I didn’t have a choice. This was what I had to take so, to be honest, I didn’t die.
I lost my hearing because of ototoxic meds. That was a choice we made, so I would not die.
Now, I can’t take cipro or any drugs in its class anymore, because my tendons are starting to get weird with it. I can’t tolerate it anymore. So that means I have fewer options for when I get sick.
I take prednisone daily. I have taken it for 15 years and I will take it until I die. It’s what’s causing all my blood glucose issues. But I can’t not take the pred. I tried to go off it. My body hated it. My joints, in particular, were not really happy. I take nexium, a proton pump inhibitor, even though I know it might cause bone issues and all sorts of other things, but reflux can lead to cancer and rejection, so, again—balancing act. I take immunosuppression meds, because I have to to stay alive, even though it ups my cancer risk by about a factor of ten, especially skin cancer.
Sometimes you start a med, have a rough few days, and then your body adjusts. Pre-transplant, I was on bactrim and cipro and a million other meds every day. At first, this was rough. Eventually, I got used to it.
The lesson here is, if you’re having side effect from a med, and it’s severe, then you need to talk to your doctor about it—especially if you’re having any sort of depression, anxiety, or suicidal ideation. Then, you must call your doctor IMMEDIATELY. This isn’t something to mess around with. Stop the med, talk to the doctor, figure out another plan! There are lots of meds out there! Find what works for you!
You have to be aware of how a med affects you. That goes back to knowing your baseline.
But yes, when you are taking a medication, your body might not like it. That doesn’t mean that it’s a bad drug. It just isn’t working for you, and that’s fine.
If you want to know the side effects of a med, they are easily google-able, or you can ask your pharmacist or your doctor. Every time I go to pick up meds, I get asked if I want to talk to the pharmacist about it. EVERY TIME. So, if you want to know, do that!
You have to know your medical history
You—as in, you yourself—must know your medical history. You must know what drugs you take and why. You must know the dosages. You must know what drugs you cannot take (if any). You have to know what is contraindicated for you.
For example: I can’t have MRIs. I can’t have PICC lines (it’s PICC, not PIC. Peripherally Inserted Central Catheter, folks.), because there aren’t any more spots for them! I can’t have zofran because it makes me vomit. These are all things I have learned and I often have to tell medical professionals these things. Because, they don’t know. Or they haven’t read my chart. (grumble grumble.)
My parents know these things as well. I have my med list and issue list on my phone so I can just whip it out in an ER or a new doctor’s office. It is a good idea to have someone else know your medical history so if you have to go somewhere in an emergency, that person can either say, yes, here’s the deal, or, “here it is on her phone.” (Now, for me, anyone who has read the book knows basically all of my medical history, ha!) I don’t expect people to be able to spout off all of it—except my parents, and they can do it—but I do have friends who know, OK, this is the deal. Especially when I travel with people, I have to tell them things that are relevant, like, me and the sun are not friends. I might have to stay inside for certain hours. I have to check my blood sugar. I might need you to get me juice. Etc.
But you have to be your own advocate. You have to say, I’m sorry, I can’t do that—and why. You have to say, I cannot take that med, or have that procedure, or whatever. (For Catholics, this also includes why you’re not taking birth control pills for contraceptive purposes! Not that you need to go all Humane Vitae on the doctor!)
Sometimes you have to talk doctors off ledges. Sometimes I get a new doctor who doesn’t realize I’m genetically anemic (I have thalassemia minor.) He’ll freak out when he sees my iron counts. But I’ve always been anemic, and we don’t do anything about it. It just is. I’m used to it!
And finally….
Be aware of change
Sometimes you’ll be on a med for awhile and you’ll be fine, and then you’ll notice…issues. That can happen. Sometimes a med builds up in your system and then it causes issues that were not apparent in the beginning. (Ototoxic meds, looking at you!) So if you have a chronic condition, you do need to evaluate. Again, know your baseline. Know what you’re being treated for. Sometimes I have to say, guys, this med isn’t working anymore. And we figure out something else.
Essentially, we all have to be aware of how we normally feel, what we’re taking, why we’re taking it, and our own health history. This enables you to be your own best advocate, which is vitally important.
Seven Quick Takes--The Medical Saga Endeth (we think)
7 Quick Takes, CF, health, hearing loss, the book1 Comment-1-
So, here’s a spicy take I wrote this week about Medicare!
-2-
And here’s the follow up:
So, we got the great folks at the CFF involved (they have a team that just looks at insurance stuff). They came to the same conclusion we did: that there really is no plan that covers everything, but that hospitals and doctors and I will make it work. (think Cinderella’s sisters: “I’ll make it fit!”) NCH doesn’t normally have a lot of Medicare people (because, it’s a, um, Children’s hospital), but….”they’ll take it”, says the finance office. (Thank you finance office!)
What I kept hearing from everyone was “well, we haven’t had to deal with this before.” Yes, I am the one that is trail blazing for everyone else. Future generations, YOU ARE WELCOME! I expect copious floral arrangements on my grave and Masses offered after I die. :-p
So, my hospitals are (sort of) covered. My main doctors—as in, the Big Three—are covered. The next issue?
The Prograf (or, THE GRAF).
-3-
The prograf is the med that basically keeps me alive. It keeps my lungs from realizing that they aren’t actually, um, the factory setting. :-D
Now, when I was emailing my nurse about this, she said, “Well, we can always try generic.”
“What do you mean?” quoth I. “Generic doesn’t work for me!”
“Well, the formulation is a lot better now, and the hospital is even considering switching its formulary to the generic,” nurse said.
AH! Well, that would solve problems!
Or….would it????
-4-
So I go to the insurance site. I plug in generic prograf, expecting to see massive cost savings and ease of access!
Hahahaha.
NO.
Generic Prograf is covered—but as a tier 4 med, meaning it’s like, non-preferred, no one wants to use it, and then I see, oh, step therapy may be applied.
Step therapy, for you new people, is when you have to try other drugs first before the company will pay for the med you want.
Yeah, we’re not doing that with the drug that keeps me alive.
So, what we’re going to do is go through prior authoritzation stuff, and we won’t have to pay out the nose, because I qualify for the Medicare Extra Help program (which is a great thing, so kudos there), so we can’t pay more than a certain very low amount.
So.
I have picked a plan. The saga is over. (For this year!)
-5-
In other news, my tree is up, and Susan the Corgi is ready to celebrate….
And I think I’m doing buying gifts. That’s exciting. :)
-6-
I had my first book interview on Wednesday with the delightful Fr. Patrick, O.P. We talked for forty-five minutes about all sorts of good stuff! The interview probably won’t be up until January, but when it is, I’ll let you know! I’ll be posting all media related to the book on the book’s page. . (And pre-order links, to a variety of retaliers, are there are well! Amazon US, Canada, and UK; Barnes and Noble; Indiebound….)
-7-
Just a note about what Kelly wrote about today—how we tell the stories of the disabled.
One of the things I’ve noticed, especially as the practice euthanasia almost on demand rises, is that people don’t really understand life with a disability, or an illness. They think they do. They imagine the horrors of it.
But honestly, that isn’t the way it works.
When I lost my hearing, it was very gradual, over a period of years. It was gradual. Now, if I’d lost it all at once, yes, that would’ve been traumatic, and highly so.
Did I grieve losing my hearing? Um, yes. A lot.
But when it came to CF stuff, it was gradual. I still enjoyed my life, and I do enjoy my life, even with insanely stressful weeks like this week.
Being disabled makes things harder, but it doesn’t make my life worthless or less.
Seven Quick Takes--the 60th of September
7 Quick Takes, Catholicism, CF, health, Seven Quick Takes, the book, transplant, writing2 Comments-1-
In case you missed it, here’s what’s been going down around these parts this week:
Simplicity Series #1—Reset Day!
-2-
The reason this post is entitled the 60th of September is because this month has seemed insanely long. Isn’t there a song called “Wake Me Up When September Ends?” That’s how I feel right now. It’s just been so long. And sort of crazy.
One of the big crazy-making things is that I’m in the middle of Doctor Roulette, which I really haven’t written about here, so I probably need to catch you up.
-3-
(If you’re not interested in medical stuff, skip this and go to point four, where I talk about BOOK THINGS!)
So, being post-transplant, and being fourteen years out, is….interesting. Obviously, I am INSANELY GRATEFUL to be at that marker. I am. Never think I’m not. But at the same time, it’s a Brave New World of Medical Stuff, because it’s rare. So when things happen, there’s not a lot of research to go on. There’s just…..talking. And guessing. And seeing what works.
Essentially, all summer we have been messing with insulin, because my blood glucose levels have been off. (I”m trying to keep this as medical jargon free, but when I say this, what I mean is my A1c, not my BGLs. If you’re confused, I can explain in another post, so let me know if you want that much detail into my life!)
So my team decided to put me on some long-acting insulin.
But……that didn’t work. First, it didn’t lower my BGLs, which I was testing twice a day, and second, insulin is a hormone. That means it can affect lots of parts of your body.
For me, that meant—headaches. Not sleeping. Weight gain (DAMN IT), and insanely inappropriate mood reactions. If Big Ben threw an interception I wanted to break things. If someone parked next to me at the supermarket, I became incandescently angry.
This is not appropriate.
And the scariest part for me? Forgetting things. Words. Ideas. What I was doing. This is not good. I rely on my brain, and words are my trade. I can’t be forgetting them! I need to be mentally sharp.
(But you’re never mentally sharp, Emily, says the peanut gallery….)
I did some digging and found out that when you have too much insulin—as in, you have WAY too much, and your body doesn’t need it—this is what happens.
And this is the problem. My body is weird. Not just the transplant weird, but weird for a CF person. I’m what’s called “pancreatically sufficient”, which is rare. It means my pancreas works like a normal person’s, not like a CF person’s. I don’t need to take enzymes to help digest my food, because my pancreas does it. I never had CF related diabetes.
And my A1c starting rising once I hit menopause—so there’s probably a connection there as well.
So, long story short, my team is sort of confused, and I’m seeing an endocrinologist the day before Halloween. That’s one reason I haven’t been writing as much this month, because things have just been crazy, but also my body has been through a lot, and I’m trying to be nice to it. Which means, chilling out, after all the non chilling out. :-P
There are some other issues, too, mainly that I don’t have a great track record when seeing endos, because they look at me and go, you’re really messed up, what do you want me to do about it?
But anyway, that’s at the end of October. Yay.
-4-
in the meantime!
BOOK THINGS!
People are starting to ask for interviews, which is….weird. I mean, good, but weird.
The cover is 99% done. I’ve seen it. I can’t show you yet. If you want to be the first to see it, subscribe to the blog!
It’s really pretty, I like it. :)
-5-
Hockey season starts soon and this makes me very happy!
-6-
I am going on retreat next week, so if you have prayer requests, I am honored to take them with me! Drop them in the combox, or use the contact page.
-7-
If you haven’t seen the Word on Fire team’s newest entries in their Pivotal Players series—Fulton Sheen and Flannery O’Connor—I highly recommend them! They’re great! Flannery is a really important influence for me, in how to live as a Catholic and a writer, and I write this quote from her at the beginning of all my journals:
I feel that if I were not a Catholic, I would have no reason to write, no reason to see, no reason ever to feel horrified or even enjoy anything. I am a born Catholic, went to Catholic school in my early years, and have never left or wanted to leave the Church. I have never had the sense that being a Catholic is a limit to the freedom of the writer, but just the reverse. … I feel myself that being a Catholic has saved me a couple of thousand years in learning to write. (The Habit of Being *)
So I love the Flannery film. It was also nice to learn more about soon to be Blessed Fulton Sheen—I had read some of his books, and I knew of him, but the film does a great job fleshing out what I knew.
(Also, in a nice twist, a college friend of mine composed the music for both films. Go Sean!)
And I really don’t think we can improve on Fulton and Flannery, do you? :) Have a great weekend!
*==Amazon Affiliate Link
Amber
CF, essays4 Comments“The Song of the Lark”
Amber has joined my buddy Sage.
It’s sort of funny. It used to be that CF kids knew each other more than I did—we’d have wards and camps and so people had lots of CF friends. I never did, because that was all on the way out when I was diagnosed. I knew one kid from my first admission—Elvis (yes, that’s his name)—but I never saw him again after those two weeks of my first admit. (Although, in a strange twist of fate, one of my best college friends was from his hometown, and his mom was his teacher.)
There was Jenny, my freshman year of college—we were on the same dorm floor. I don’t know what happened to her.
But post transplant, I met more people with CF. Sage. Piper. People on Facebook. Kathleen. And Amber.
Unlike Sage, I had met Amber several times. She was the second transplant at our center (I was first, a fact that was a bee in her bonnet for awhile. Cracked me up.). She was younger than me, around my brother’s age (she was born in 1986). She’d been diagnosed with CF the normal way—as a little kid—but she lived nearer the Toledo center so that’s where she got her CF treatment.
We were both writers—she wrote a book called Breathtaking about her experience—and we both went to small Ohio colleges. (She had started at Cedarville University, but couldn’t finish because she got too sick, and eventually graduated from Moody Bible College.) She had a husband and they had adopted a little boy named Noah. He started preschool this month.
Amber had been in rejection for about two years, but she was a force. I mean, I’d never met anyone who was so unapologetic about herself, her life, her goals. She just told you whatever she thought, right out. “You can’t say that to people!” I”d tell her.
“Why not?”
Eventually, some of this rubbed off on me in dealing with our doctors. Ha.
She was just so unapologetically her. Honest, open, passionate, feisty. You always knew what she thought. But she wasn’t mean. She was just open in a way that a lot of people aren’t.
For two years she’d been driving from her home in northwest Ohio to get treatments at The Resort, to try to keep herself alive. There was talk of listing her for a second transplant.
I last saw her in July, at clinic. Clinic days are Mondays and so generally you tend to see other pre and post transplant patients at the same time in the halls and labs and in outpatient radiology. We got to catch up a bit, which was nice, because we hadn’t in awhile. She was carrying around a portable oxygen tank (when I say portable, it really was—it could be slung over your shoulder like a purse), but she was still fiery. Still giving me crap for wearing a skirt to the doctor’s. :-p “Comfort!” She said. And she was right, but I told her I preferred to use my feminine wiles to make the doctors do what I want. I was kidding, and she knew it, and we laughed about it.
I had seen on Instagram that she had missed an outing with her son to the zoo on Labor Day. But I thought she was okay. I have a news feed filter on my facebook app—basically, i don’t see scrolling updates anymore—so I had completely missed that she had been admitted with pneumonia and they had bronched her and she was in the ICU while they figured out a long-term plan.
I messaged her on Wednesday, to ask her a question about treatment. It was my brother’s birthday.
I got from his birthday dinner that night to find a message from her husband—Amber had died on Monday morning.
*
I don’t know why I’m alive, still, and Sage and Amber aren’t. Part of it is the idea that their journey, what God wanted them to do with their lives, was “complete”, I guess. And I’m not done. Which, I mean, is fine, I like being alive. But why me? Why not them too? Why are their husbands widowers, why is Noah without a mom, why did George the dog never see Sage come home? Why? Why do my siblings get to have me, and their siblings don’t?
I don’t know. I know God knows, I know He has his reasons, but I don’t know how much that really helps right now.
In Amber’s case, she had almost fourteen extra years. Her transplant anniversary was September 25. In those fourteen years, she wrote her book, she traveled to speak, she got married, she adopted Noah. She had extra time that she never would’ve had other wise.
But she was still only 33. Sage got an extra year of life, she had a wonderful husband and family and the sweet pups and even sweeter nieces and nephews.
I’m older than both of them.
A lot of people, post transplant, experience the feeling that they need to live for their donor. That they’re sort of entrusted with continuing the donor’s life as well as their own.
I never really felt that—probably because my donor was older, so it wasn’t like another 23 year old had died. (I’m not denigrating my donor’s gift, obviously! OBVIOUSLY. Just trying to explain how I feel.)
But I do feel, now, like I’m living for them. Sometimes I know Sage wants me to do something, to be brave and to ride it out.
And now I’ll feel Amber yelling at me to be honest and tell them how I really feel and figure stuff out, dang it. To just do x.
Both Amber and Sage had strong faith. I know that they’re happy. (I mean, one has to be happy when beholding the beatific vision, right?)
But gosh, I miss them both.
Doing The Best You Can With What You Have
CF, health, transplant1 CommentUnder the Wave off Kanagawa (Kanagawa oki nami ura), also known as the Great Wave, from the series “Thirty-six Views of Mount Fuji (Fugaku sanjurokkei)”
I was talking to a friend of mine the other day, who, like me, has had some health problems. And we were talking about how the things you do to save your life can later come back and have unplanned consequences.
“I’m dealing with that right now,” I said. We talked a bit more about how frustrating this is—but then we asked, Would we have changed anything?
And the answer is, probably not.
So I thought I’d write about this.
*
After my clinic visits, we always have to wait for blood test results. One of them that we’ve been watching lately is called the A1c, which I talked about in the last post. Basically, it’s a batting average for your blood sugar. And ever since I entered menopause it’s been going up….and up….and up.
This is not good. The more sugar is in your blood, the more that can lead to lots of problems. Problems that I don’t want.
This isn’t CF related diabetes, because my pancreas still works. (I don’t take enzymes to digest my food, so that’s how we know….) But at the same time, my body is clearly becoming insulin resistant.
I’ve been on steroids for 14 years. So the thought is that steroids + menopause=unhappy A1c.
Now, I can’t go off steroids. I’m on a low dose—5 mg a day. There is a 2.5 mg dose. And I might try that. But the problem is, my body has adjusted to them, and my joints, especially like prednisone. A lot. I had CF related arthritis before my transplant and that is helped a lot by the prednisone. I notice when I miss a dose. So when I tried to go off prednisone a few years ago, my body said, “nope.”
Why am I on prednisone? Because I had a transplant.
Which saved my life.
But we know that prednisone has a lot of side effects.
*
Another area where side effects come to play? Cancers. We’ve talked about that a lot here.
And, not pred related, but med related—my hearing loss.
So, these are all things that have happened as a result of staying alive.
But—what were my choices?
Well, to take the meds, or die. Really. It was that stark, in a lot of cases.
So I decided to take the meds. And live with the side effects.
And that can be sort of sucky, to be honest. Because you do things to save your life, but then…there are consequences, and you have to be ready to deal with those. It’s a long-term gamble.
But, and I said this to my friend, we do the best we can with the information we have. We can’t think about 5, 10, 15 years down the road when we’re looking down the barrel of the gun right now.
If you’re in that situation, I know how you feel. I know it’s hard not to google and think about the future. But really, in my opinion, the best thing to do is to talk to your doctors, see what the options are, and then go with what is best—for you, for the situation, for what needs to happen to achieve a good outcome.
Does that mean you’ll be thrilled with what you have to do? Well, no. I’m not thrilled that I’m injecting myself with five units of insulin every night. But it could be worse.
This is what I have to do to stay alive—to see year 15, year 16, year 17….post-transplant.
Now, are there things I won’t do? Yeah. I’ve always said I wouldn’t go for a third transplant. That, to me, is a bridge too far.
But right now, I take the insulin, I adjust my diet, and I do the best I can with what I have.
Day In the Life: Yearly Transplant Testing
CF, health, transplant1 CommentI thought that I’d give you a little glimpse into a day at clinic, but in order to get the most bang for your reading buck, I chose do chronicle a day where I do yearly testing—as in, clinic, blood draws, X-rays, CT scan, and a DEXA (bone density) screening. So come along with me on Monday’s trip….
6:30 am: Alarm goes off.
7:20 am: Out the door, to the hospital!
It’s not raining! Yay!
The hospital is only 12 miles away form my place, so that makes it easy to get there, but morning rush hour can be a beast. Fortunately, it’s not bad, and I get to the parking garage at 7:45, after being asked for the nth time if I’m a visitor. No, I am a patient. Deep sigh.
Excellent parking!
The hospital has a nature theme, so there are lots of animals and other nature-ish things around. In case you can’t tell, those big green things are acorns.
7:50: Heading to Crossroads Registration
dooooown the long hallways.
I passed this bunny on the way in:
Registration is in the middle of the hospital complex and sometimes it can be a pain. But there was a nice lady behind the desk, the kiosks worked, I had my wrist band, and was on my way to infusion for my first appointment….
Up we go!
The tower building used to be the main hospital—I’ve spent a lot of time here. :) The fourth floor (4AE) where infusion is is where the adult CF floor used to be. It’s where I almost died and it’s where I waited the night my transplant came.
The 4th floor is also home—or was—to the PICU. So yeah, the fourth floor has lots of great memories. (Seriously, some are good. Most are….not.)
It does, however, have a good vending machine.
Anyway!
8:00 Infusion
In the waiting room—Muppet Babies on TV.
Great view, huh?
Since I was early, I got taken back early—yay!—into one of the rooms. Like I said, these used to be patient rooms. Now they’re smaller. Most of infusion is separated by walls and curtained off areas, but since I’m a transplant patient I go into an actual room.
Sometimes infusions last for hours. Really, the reason I go to infusion isn’t to get meds, it’s to get my port accessed for blood draws. So the room has a bed, and the other areas have recliners, if you’re staying. I’m not. This is an in and out thing.
My great nurse comes in and sets things up….
Fortunately no vitamin levels today, so only three tubes. We could not get that out of my veins. So—port!
The blurry part is the strips that have my ID number on them and get attached to various things when the blood goes to the lab.
And yes, everyone must wear PPE—personal protective equipment—when they access the port. Gowns, gloves, masks, and hair nets. It’s like we’re doing surgery here.
So, we’re running ahead of the game, but then my port decides to be dumb, so we have to wrestle with it for ten minutes, but finally it cooperates and we get the blood. Then we flush the line with saline and heparin, and de-access me. Yay!
I am free to go back down to the main floor!
Hallway out to the waiting room.
Doooown we go.
This used to be part of the old ER—the parking lot to the right is where we dropped me off the night of my transplant.
(Bunnies ahead!)
This used to be “main” radiology, and the little hallway you see above used to run between radiology and the ER. This also used to be the main hospital through way—if you went to the end of this hallway you’d reach the main lobby. But I digress!
I’ve been coming to this part of the hospital for twenty-six years. It’s very familiar.
As is this hallway, but now they’re changing it! I don’t know what to do ! :-p
8:40 AM: Chest X-ray
So I have my probably five millionth chest x-ray (that’s a conservative estimate), before which I ran into my post-transplant buddy Amber, who is also going to clinic. It’s always fun to see friends!
So, out of radiology, heading toward clinic, and passing the fish tank and the satellite gift shop.
(Yes. There are two gift shops)
Sharkbait!
Past the coffee bar….
To the elevators, and up to good old fifth floor CF clinic! :) Also been coming through this door for 35 years. :)
9:00 AM: Clinic
This is where I spent the bulk of my time. On a “yearly” clinic day, everyone comes in: the doctors, the dietician, the social workers—and things get a little more in-depth. (Not so much on the doctor end, since I see him every three months.)
*The dietician asks me to talk about what I normally eat: meals and snacks. She’ll then give suggestions. Right now, we’re dealing with weight loss and the silly A1c levels (more on that in a bit), so we want to make sure I’m eating the right combination of things. She made some suggestions, I asked some questions, and it took about a half hour, probably. I really like the dietician so that helps. :)
*My Doctor. I see one of the two docs on the team every three months. This time, he was happy with how I was doing, and we talked about the A1c thing.
Basically, the A1c is a test that looks at how your blood processes sugar all the time—it’s like a batting average. It’s how much sugar “sticks” to your red blood cells. For normal people, you want it to be under 6% For post transplant people, you want it to be in the low 6%, because the prednisone we’re one messes with how our bodies process sugar. So we aren’t aiming for normal people normal, but abnormal normal. :)
I had been testing my blood glucose levels (BGLs) for a few months, and my doctor didn’t think my numbers were really all that bad. (Again, we’re looking at abnormal normal here. Not normal people. ) He did say that if my A1c was up, then we’d probably have to start me on a low-dose, long-acting form of insulin. It wasn’t really because I hadn’t done what they asked—I lost weight, I’m being more active, and I’m checking my BGLs—but because I’ve been on prednisone for 14 years, and I’m in menopause, which, as we know, messes with hormones like nuts.
But my Chest X-ray looked good, and my PFTs were up a point, so lung wise, things are great. Sinus wise, things are great. I’m seeing all my specialists like I’m supposed to and I keep clinic informed of things there.
My doctor wanted me to do some other PFTs so I had to go back to the lab, but we’ll get there in a second. :)
*Social Work: Normally, they just come in and ask how I’m doing and give me a parking token. Since I’m working with some insurance insanity right now, we had more to talk about and they are going to look into some things for me which is massively helpful. So I was happy!
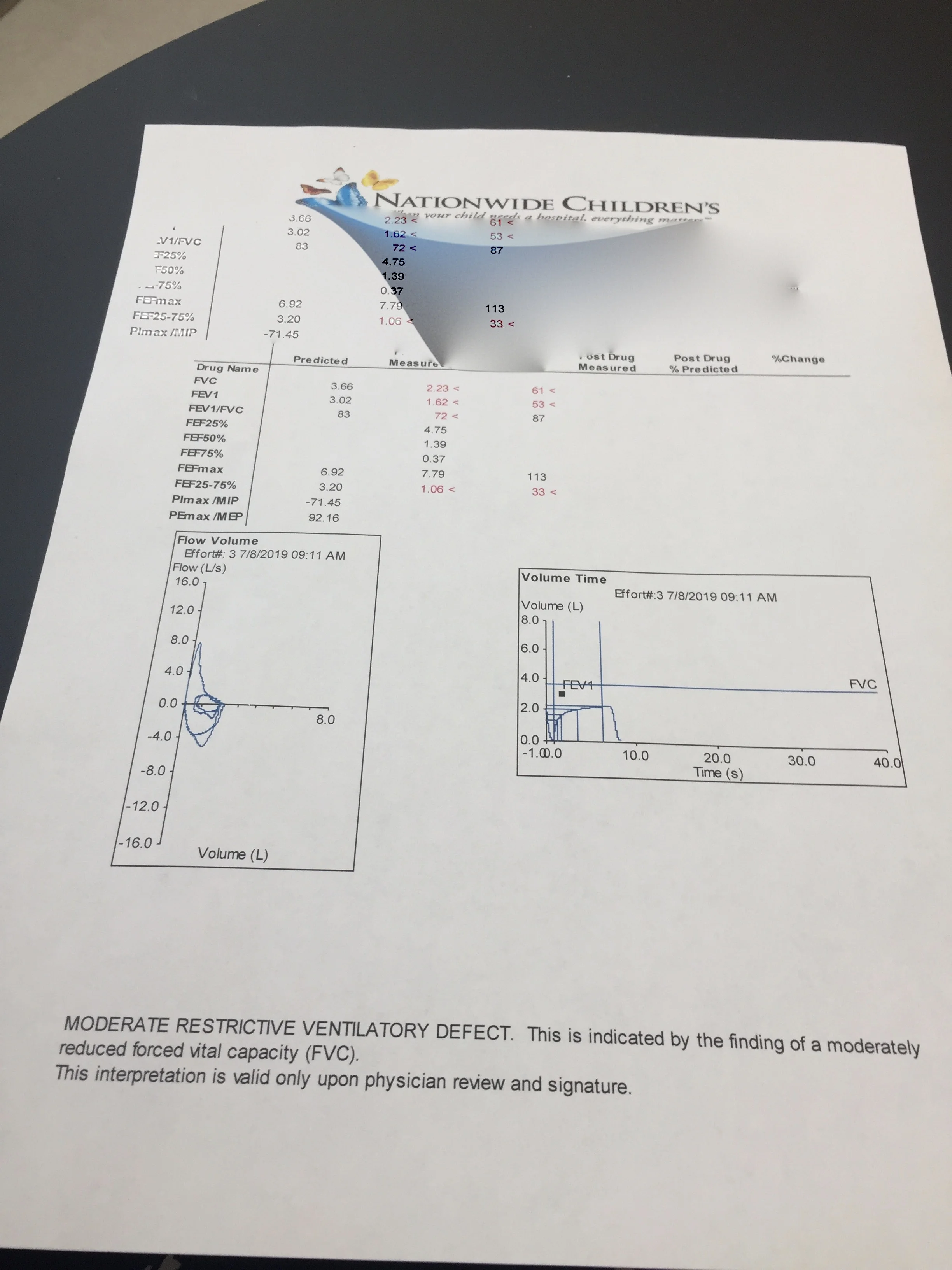
Finally, Pulmonary Function Tests, aka, PFTs.
Normally, when I say I’m doing PFTs, what I mean is I’m doing spirometry. Aka, the thing where you sit down, put clamps on your nose, and breathe in through a tube connected to a computer. You breathe easily for a few breaths (for me it’s two) and then on the third you take in a huge breath, like you’re about to go underwater, then blow it out fast and hard.
You then get results that look like this:
swirly bit is blocked out personal info. :)
Now, this is in liters, and I generally look at percentages. As of yesterday I had about 54% lung function, which is good for me, and that’s the “moderate restrictive defect” part. It’s not anything to worry about, it just says that at the bottom.
I also did two other kinds of tests which check how gases are diffused in my blood and other breathing related things. Those were also fine. So yay there.
11:00 Finished clinic, back to radiology!
I finished in clinic, said goodbye, and my nurse said she’d email me with follow-up things. I then headed back down the elevators,
past the fish….
And back to radiology.
This was a bone density scan that did scans of everything—we did hip focus and lumbar focus, and then the whole body. This is important because prednisone (don’t we love it?!) also causes issues with bone density and causes osteoporosis. Fortunately my bones are AWESOME. I hope they continue to be awesome—I haven’t gotten these results back yet.
FINALLY, the LAST TEST!
11:45 am: Chest CT
so heading back through the center of the hospital, to the Magic Forest!
And into the CT room:
This is just a regular old CT scan of my lungs to make sure we’re not missing any small things that might be happening that regular X-rays don’t pick up. Easy peasy.
So I was free, and said goodbye to the bunny, at around 12:15!
I was really hungry at this point, because I’d only had a little breakfast—you’re not supposed to eat a lot before clinic visits in case something scary shows up in testing and you have to have a bronchoscopy that day. (Yes, that has happened to me before.)
So I was hungry and had walked about a mile and a half, not kidding, in the halls of the hospital. I hit my move goal for the day at 3 PM, so I knew that I’d get a decent workout on this day, lol.
This used to be a longer day—there used to be more tests. So I’m fortunate that this was a pretty quick day and everything went well, except for the silly port being stupid! :)
Joy In the Morning (OR: How I get up every day and do life)
CF, essays, transplant2 CommentsMy siblings and I on my brother’s wedding day.
Warning: This might be a sort of rambly post. Settle in.
I was visiting my therapist last week. Yes, I see a therapist. I have since I was 17. A lot of people with CF do (not all, but a lot). I have no shame in telling you that.
So anyway, I was at an appointment with my therapist, and we were talking about how I was a bit maxed out on doctor visits. I mean, in almost thirty-seven years of life, I think my quota’s been hit, right?
And that doesn’t even count the other “stuff” we do—Mom accessing my port every month, the meds I take (which are vastly less than pre-transplant, btw), the blood glucose tests I’m doing twice a day now, etc. It’s a lot. It’s less than pre-transplant in some ways, and more in others. I have a colonoscopy every five years, which means one next year. I have a mammogram in April, because my mom had breast cancer and so my sister and I have to start our mammograms at age 37 (ten years before Mom was diagnosed). And then there’s dentists and eye doctors and the things normal people do.
So, yeah, it’s a lot.
This led to talking about compliance, which means, doing what the doctors tell you to do. And I told a story that I thought was illustrative.
When I was about seventeen, I was having a regular clinic visit, an I saw a sign on the wall of the exam room, saying that if you were 95% compliant with taking pulmozyme (one of the CF meds), you’d get a prize at your next clinic visit, see your nurse for a chart to win! Stuff like that.
Now, I never did these, because, generally, I was too old. This stuff was generally for the smaller kids, to get them in the habit. But what I thought was interesting was that the center wasn’t pushing perfect compliance.
Because that doesn’t exist.
Now, look, I’m not saying I was a slacker. Because I wasn’t. My mom, for one, wouldn’t let me be, even if I was disposed that way. I take my meds. I did my treatments. But yes, sometimes there were times where I put in a few minutes of precious sleep over a “perfect” Vest treatment, when I was in college. Sometimes I just went to bed. Not often, but sometimes. I wasn’t “perfect”, and I’m not perfect now. To be “perfect” now, I’d be a MESS. I’d be taking meds all day long, worrying about timings and if this was going to interact with that and how does this work and oh my gosh my brain is going to explode!
I take all my meds, and I take them twice a day. Is that perfect? Well, no. It’s not optimal. If can affect absorptions. *
But here’s the thing—I want a life. I don’t want to live in a glass bubble.
I went to school. I did activities. I rode bikes with my friends and went to the pool in the summer with them and then we went to the coffee shop and played board games. I had sleep overs, where I didn’t bring my equipment! I went on choir tour! (And yes, I brought the mini nebulizer!) I went to college.
Honestly, if my parents had tried to wrap me up in the bubble, I would’ve had a fit. I always wanted to be like everyone else, as much as possible. As Erin once said in a Home Town episode, I’m like a wild pony, and I need freedom!
(Not too much freedom. But enough freedom.)
So anyway, talking about all the things I had to do every day, my therapist then said, well, how do you do it? I mean, what gets you up in the morning?
And then I said, “well, that’s sort of what my book is about.” (Because it sort of is. Sort of. The book is sort of about a lot of things! )
But here’s what it comes down to:
Yes, there are a lot of things I have to do in my life. More than the average bear, that’s for sure, so when people say “well, you just have to suck it up and do X,” I want to roll my eyes, because that’s a big chunk of my day. (I’d wager it’s a large part of everyone’s day. As my grandfather used to say, “that’s why they call it work!”) But yeah, for me, and for other people like me, we have a lot of stuff on a daily basis that isn’t fun but must be done, and you just do it and don’t whine about it.
But what gets me up in the morning? Well, a lot of things. I’m very in touch with my inner child and I get excited about really little things. When I was working in the Senate, a lunch date with my Dad was enough to make me excited for the day. Today, it’s stuff like, a package is coming in the mail! It’s a hockey night in Pittsburgh! I get to write today! Oh, this book comes out! My book is in at the library! Chuy’s with Mary!
I’m very easily amused. And that helps me, I think, because it overrides a lot of other things that are not so fun. (Like making myself go to the gym. And poking my fingers. And doing doctor paperwork.)
But a big part of this, and this is what I’d say to anyone facing a chronic illness, is this:
Go live your life!
You really, really, really cannot hole up in your house and be all sheltered. You can’t. GO LIVE YOUR LIFE. Go outside! Do things! Be free! Have fun! Go to the park! Go swimming! Pet a dog! Whatever!
Yes, treatments are vital. YES, compliance is important—if I hadn’t been a compliant patient I NEVER would’ve been listed for transplant! But if you’re caught up in PERFECT, then…..you’re going to miss things and your life will be so small.
Seriously. Do what the sign says.
Live your life. Take your brain with you.
*: As far as absorptions: the only meds I take that NEED to be taken around the same time every day are my immunosuppressants (the prograf). That’s important. However, I am also far enough out that if I’m off by a few hours in a dose, the world will not end. When I traveled to LA, my nurses told me to just take the meds on LA time and not worry about being exact. I used to take my meds exactly at 8 AM and 8 PM (even rushing to the lobby of the Ohio Theater to take meds before a symphony concert started). Now, it’s generally around those times. I’m not quite as OCD.
The meds I’m talking about here are things like my nexium and magnesium supplements. You’re not, really, supposed to take them together. But if I didn’t, then I’d be carrying around meds all day and thinking about when to take them, as opposed to thinking about things more worthy of my brain space! It’s not a huge deal to take them together. But yes, some meds do have to be taken at certain times, and when I do those (like home IVs) then, yes, it’s on the dot as much as possible. You usually have about an hour leeway on either side of the dose time (for example, if the dose is due at 6 PM, you can do it at 5 or 7, but not 4 or 8.)
On My Soapbox: When people say they want "healthy" kids
Catholicism, CF, essays, health, life issues, transplant3 Commentsand some theology
I know that when most people say they want a “healthy baby”, they’re not being rude or mean. They’re probably trying to be nice.
But guys, I wasn’t a “healthy baby.” I looked healthy, initially, but I wasn’t. I had seizures. I had (and still have) thalessemia minor (I think it’s called type b now? Not sure). I got the CF diagnosis when I was 11.
So, should my parents have just pitched me back? “Nah, sorry, we wanted a non-defective model.”
And I know that people do that now. People kill their babies in the name of the kids “avoid suffering” in their lives. Bull crap. “Yes, let’s kill you, so you never get to have a life.”
That ties into part two: saying “God is Good” only when things go the way you want them to go.
Guys. God is good all the time. He is Good. It is in His very nature to be good. But that doesn’t mean that God’s Goodness=what you want.
Because it doesn’t work that way.
God created me with my “defective” genetic code and my blue eyes and my blonde hair and my fair skin and my wonky teeth and an ankle that cracks oddly. I have a really good memory and I love children and I do a pretty good Sebastian the Crab imitation. I have The Phantom of the Opera libretto memorized. (And Les Miz. And Miss Saigon. And Ragtime. And Parade…)
And yeah, I also have CF. I had a transplant. I’ve got scars. And I do talk about it, because it has become clear to me that it has to be talked about, because people see illness as scary and something to be avoided and pain as awful, to the point that Canada is allowing pediatric euthenasia.
God is always good. And God made me the way I am for a purpose. Is it always fun? No. It is not. There are times when I’ve been really peeved about it, to put it mildly.
But at the same time, it has made me who I am, and in general, I like who I am. I wouldn’t want to change that for the world.
God is not being “mean” to me. He created me the way he wants me to be.
And health doesn’t always stay health. Health is a transient thing, guys. Everyone will get sick. Everyone will die. It seems that in our society now we are idolizing life and health to the point that it is fully unhealthy. We’ve forgotten that we will die, that life is fleeting, that our home isn’t here.
Children are a gift from God, no matter how they come.
And God is always good. And He always loves me.
He always loves you, too. No matter what.
As [Jesus] passed by, he saw a man blind from birth. His disciples asked him, “Rabbi, who sinned, this man or his parents, that he was born blind?” Jesus answered, “Neither he nor his parents sinned; it is so that the works of God might be made visible through him.”
Med-sanity II
health, CFCommentMy coffee machine died yesterday. It was speedily replaced, so let’s think about the wonders of coffee and lovely rainbow colored tea tins from David’s! :)
I was supposed to have a procedure done on a skin cancer on my ear today, but that’s not happening. Because….sigh.
A little background. While CF is becoming less of a “childhood” disease and more of an “adult” diseases, adult hospitals have not caught up. I’ve been in several, and what I’ve noticed at 98% of them is that the doctors and staff cannot look at someone “young-ish” and see chronic disease. They think that anyone under 50 must have been perfectly healthy her entire life and thus, can just do whatever they want.
WRONG.
A few examples:
You can’t do an MRI on me. Magnet in my head.
You can try to put in a PICC line, but it won’t work. My veins are all scarred over from the years of previous PICC lines.
You can’t use adult sized needles on me; my veins can’t take them. You need baby sized needles, small child sized needles. I have small child sized veins. And you also have to be good—you can’t just look in the crook of my arm or my hand like you could with a regular adult. I’ve had IVs in my shoulder. I’ve had them in my thumb.
And, what’s pertinent to today’s discussion: I am on many* meds for a variety of conditions. You can’t just prescribe a drug for me without looking at side effects and being aware that they might happen.
This is relevant because, as I wrote in the previous post, when you already have mental health issues, you tend to not like drugs that can make those worse.
So, when I (my mom) called the doctor about the side effects I was having—supreme irritability, mood swings, etc.—the nurse said, well, stop the med and I’ll talk to the doctor.
OK. Done.
We (mom and I) get a call a few hours later when we’re at dinner. The nurse says that 1) the doctor doesn’t think the med is causing the issues, but stop anyway 2) they cancelled my appointment for today and 3) they want me to go to my “PCP” (primary care physician) to have my “mental stability” assessed.
That last point is sort of an insult, frankly.
I’ve been seeing a psychologist since I was 16. I’ve been on a medication for anxiety for that long. My doctors KNOWS this. It’s in my freaking chart, that I take this med. I am not unstable, but yeah, the med you put me on? Made me a littleeeeeee irritable and sort of unhinged. Yeah. But that doesn’t mean I’m going to flip over procedure trays and get into WWE fights in the waiting room. Stop the med and I’ll be fine.
It’s like when I do a steroid bolus. It makes me SUPREMELY cranky and irritable. But I know it’s the meds and the courses are usually short. In this case, the med isn’t even necessary, there are other ways to treat this guy. I’ve had lots and lots and lots of terrible medications in my life that have given awful side effects, but they’re necessary so I suck it up and deal with it. This isn’t necessary.
Second, I don’t have a GP/PCP. I TERRIFY GPs, because I’m complicated. The ones I’ve met are usually afraid to do anything to me because they don’t want to mess things up. So my “GP” is my transplant pulmonology team.
Third, read my freaking chart. Really. It comes back to this all the time with adult hospitals and physicians. “Do you have lung issues?” Seriously, I was asked that question. (Not by this doctor. Another wonderful adventure years ago.)
So a procedure today had to be rescheduled for next month, and I have no idea what we’re doing with the cancerous spot on my arm, except I’m not taking the med anymore to treat it.
Which brings us to the big lesson, here:
I have lived in my body for 36 years. I have a very, very well-tuned—exquisitely well-tuned, I’d say—sense of status within it. I know when “something is not right”, to quote Miss Clavel. And I don’t think I’m exaggerating when I say that that instinct, and my parents’ equally honed instinct, has saved my life on a few ocassions.
Doctors and medical people need to listen to me. I’m not always right. But when I say something is the med, it’s the med. When I say X is happening, and it’s because of Y, it probably is.
It’s basic science. When you do an experiment, and you add a variable, an things go haywire—it’s not because of everything that came before. It’s the variable you just added. That thing has pushed the balance over the edge. Remove that thing—balance restored.
*I am on vastly fewer meds now than before transplant. That being said, I’m still on what the average person would consider “a lot” of meds.
Sage's Shawl
CF, essays, yarn along, knitting, journal2 CommentsYes, it's Wednesday. It's a yarn along post. But....not really.
When I finished my first Drachenfels shawl, I knew I wanted to knit it again. My head was full of color combinations and possibilities. In May, I ordered a special edition yarn from Quince and Co (carnation--the pink above) and knew I wanted to use it in this shawl. The question was--what to pair with it?
When I went to Sewickley Yarns in July, I brought the ball of carnation yarn with me so I could color match. Immediately, I latched on to the green color you see above. And then I checked the tag.
It's called "Sage".
Then I knew I had to have it.
Some of you may remember my friend Sage, who died two years ago Friday, waiting for a double lung transplant. Like me, she had CF. And we had so much in common besides that. She was a true kindred spirit. We spoke (well, texted) almost every day. She was funny, supportive, deeply faithful, and just....well, a perfect friend.
We never got to meet, but we had made plans for it...in that nebulous future moment of "post transplant", the transplant I was just so sure she'd get.
She didn't.
I think about her almost every day. I think of things I want to tell her and then I realize I can't.
So when I saw the "Sage" yarn, I had to get it. And then I had to get the purple (Frank's Plum), because purple was her favorite color. It's also the color for CF awareness.
I wish I could give her this shawl. I think she'd like it. I know she'd love the purple. I dunno how she felt about pink. But since I can't give it to her, I make it for me--and when I wear it, I can remember her encouragement, her sense of humor, her strength (really, she was so much stronger than I am. Anyone who gets a chest tube put in WITHOUT ANESTHESIA is MUCH stronger than I am.).
Some people, post-transplant, talk about living for their donor. I never felt that way. My donor was a lot older than I was, for starters, so it wasn't like she was a compatriot in age. But after Sage died, I do get the feeling that I'm living for her. That I do some things because she can't. It's hard to explain.
I'm at the halfway point of the shawl. For the rest of it I'll be working with the pink and the purple intertwined together. I should finish it within the next few weeks, which means I can wear it this autumn.
So, if Sage was alive, I'd give this to her. But since she's not here, I'll wear it for her.
Thirteen
CF, family, essays, organ donation, transplant1 CommentThe annual transplant anniversary post tends to change, in form and shape, every year. This year, a lot has happened:
Catholic 101 was published in November (buy it here--on sale until Friday!)
My brother got married
(c) Erica Kay Photography , http://ericakayphotography.com/home
My sister got engaged
Melanie and Jason (her fiance) leaving Bryan and Sarah's wedding (c) Erica Kay Photography, http://ericakayphotography.com/home
I saw the Stanley Cup with my parents
I went back to Williamsburg and Duck
I started writing and editing for Take Up & Read.
I celebrated my grandma's 88th birthday with my family
I knit my first shawl.
None of these things would've happened without my donor.
It can be tempting to look at life in terms of productivity, what we do, and I'm not trying to list my productivity. Look at what I've done! Rather, it's more like, these are things I never would've done, enjoyed, even conceived of, thirteen years ago. These are things that never would've happened.
I would've missed my brother's wedding.
I never would've met my new future brother-in-law and sister-in-law.
13 birthdays, Christmases, holidays....all those things would've passed without me.
In general, women post-transplant don't do as well as men. There isn't a lot of data, period, on women who have survived a transplant longer than 10 years. I'm in new territory here.
I try not to think about that.
Instead, these things I get to do are gifts, even when life is sort of sucky, because life is never totally perfect. I mean, things are overcome, yes--but just because something is overcome doesn't mean that everything is suddenly perfect. It doesn't work that way.
Someone said, life is full of suffering, but it is also full of the overcoming of it.
And that about sums it up.
Thirteen years of overcoming is pretty good.
With the cousins on my mom's side at my brother's wedding. This is not all of them, btw!
To be an organ donor, go to donatelife.net/register
The Big Bad Wolf
CF, essays, health, transplant2 CommentsI’ve had depression and anxiety issues since I was 15 years old.
Maybe I was born with them and just never really had an episode until I was 15, and I had a TB diagnosis that came really late and almost killed me. “This is just what CF is,” said a doctor in my CF clinic. But when I started coughing up blood, my regular doctor decided to look a little deeper, and she found I had non-infectious TB, something that only 4% of the CF population ever gets.
So it was a brush with death that hit a little close to home. TB is called “consumption” for a reason. It consumes you. The meds made my stomach hurt so much that eating made me cry. I cried thinking about eating ice cream. Who cries about eating ice cream?
The TB seemed to awaken this depression and anxiety in me. I became afraid of the dark. I had no energy, no interest in anything. It was the only marking period in my high school career where I didn’t make the honor roll (and you needed a 3.0 to make the “basic” honor roll). I stopped voice lessons.
I don’t know if many of my friends noticed, but it took awhile to get over the feeling of intense worry and doom (and that’s not too strong a word) that hung over me. As spring and summer came, I slowly got better, both physically and mentally.
Of course as my body recovered, that helped my mental health recover too. The two are linked. But what also helped was my fabulous doctor discerning that I probably needed some additional help, in the form of both a psychologist and medication.
She approached it very gently and made it clear that it wasn’t a mandate, it wasn’t that something was “wrong” with me or that I was “crazy.” She thought that it would be the best way to keep me healthy going forward, and she was right.
I’ve seen my therapist regularly ever since--that’s more than twenty years now, with the same woman. She’s not allowed to retire, ever, basically.
But I’ve also taken medication. It’s changed, over the years, because of drug interactions. But I need it--I can’t go off it, or I get a little unhinged.
I should probably describe what “unhinged” means for me. It means that I start worrying about everything. I feel like I’m a burden to everyone, that nothing is going to go right, that my body is my enemy. I have trouble breathing and have a lot of chest pain. Now, as I say that, I can differentiate between the Big Bad Wolf of anxiety/depression as opposed to the chest pain and troubling breathing of a pneumonia or lung infection. They are different, and I can tell said difference. Some of that is just being older and learning how my body reacts, and what else is going on.
If it’s emotional, then I’ll be very withdrawn. I won’t want to go out. Everything will be much harder than it should be. I will be cranky and cry at the drop of a hat. I won’t want to leave my house, get dressed, or do anything other than sit on the couch. I won’t even want to read.
It’s not good for me to be in my head that much.
And the other thing I’ve noticed is that most people get seasonal depression in November/December. For me, it’s right now--it’s June/July. This time of year is not a good time of year for me. Maybe because I’ve had a lot of home IV bouts, hospital stays, and work stress in early summer. Last summer I noticed this for the first time….I really don’t like June and the beginning of July. But after the beginning of July, around my transplant anniversary, things start to lift.
I don’t know if it’s PTSD or what. I hate to think it is PTSD because I honestly don’t think of my life as traumatic. But whatever it is...I know it now.
So I’ve talked to my doctors and we’re upping my medication dose for a little while, until I get over this patch. It’s helping already--so that was fast.
I don’t react well to lots of stress, either--so when you combine stressful events PLUS this time of year, it’s really not great.
And part of it is I need to be less nice. I need to stop worrying about making everyone else happy and worry about making myself happy, or, at the very least, healthy. That’s gotten me into trouble before, the idea that I have to do everything even when my body says no. I have to stop letting other people’s expectations dictate what I do--and that’s a lot easier said than done.
I hate to let people down. But at the same time, if I was honest with people, then I bet they wouldn’t want me to run myself into the ground and into the black hole for them, because there’s nothing I do that’s really that important. Let’s be honest. I’m not running the world here.
That’s one thing I want to say to people who struggle like I do: life is not an emergency. (Thanks, Ann Voskamp.)
You are not running the world.
If you have to take a day off, you can do it.
But you have to be vulnerable and tell people that.
And that is hard.
I know it’s hard.
I’ve wanted to write this for awhile, but I’ve been afraid of what people would think or say or how they’d view me.
But you know, we need to be honest, guys.
We need to bring this stuff out into the open.
There are not enough people talking about depression and anxiety and how we just deal with it every day.
We talk about cancer and everything else, and I talk about my transplant.
But sometimes we need to talk about this stuff as well.
Because it happens to everyone--those with faith, and those without. Single and married. Poor and rich. Every color, every race, male and female.
So, here we are.
I’m writing about it.
And I hope that this helps someone, even marginally.
I look really happy most of the time. But that doesn’t mean I am happy.
Sometimes it’s all too much and I need a break, but there’s a difference between a break that I call for rationally, and a break that is imposed because my mind is going five million miles an hour and I just need to clear the decks.
In fact, that’s a good description of what my medication does. It helps me clear the decks and be rational and logical and awesome.
I think I’m going to write a few posts about this. This one is a good starter, a good ice-breaker.
The take away is this: Get help. Ask for help. Be honest and vulnerable, and you’ll be surprised at how people will support you. (If they won’t support you, then you don’t need them in your life. Full stop.)
For me, this was the hardest part. Being vulnerable is NOT something at which I am good.
But it’s worth it.
Stop waiting around
CF, essays, transplantCommentTrivia night victors!
Guys. Stop waiting to do things.
I see this a lot with transplant people--or people with CF--but also with people who are just nice, normal people.
"Oh, I'll wait until later to do that."
"Oh, someday...."
"Oh, it's just not right right now."
Guys.
If you want to go to school, go.
If you want to learn something, learn it.
If you want to bake cookies all day, do it at least once.
If you want to learn Spanish, sign up for Duolingo.
STOP WAITING.
Stop saying, Oh, when this happens.
Nuh uh.
DO IT NOW.
Yeah, sometimes it's not plausible. I get that. Sometimes you have to save money. I get that too.
But then DO IT. Save the money. Make it happen. Dedicate yourself to it.
Don't wait.
Don't use your body as an excuse not to do things. "Oh, I have crappy lung function, I can't go to school, I can't work, I can't do anything by lie here and watch Netflix."
I've been there. Before my transplant, I slept for 13 hours a day. Seriously. If not more. When I was "awake", I was sort of zombie-fied. And that's what happens when you're close to death.
But EVEN THEN--I went to work. I went out. I saw my family and friends.
Yes, when life changes, more opportunities can open up.
But you will lose your life waiting around for things to happen.
So STOP IT.
Learn the things. Do the things. LIVE YOUR LIFE. Even if you're almost dead, you can STILL LIVE YOUR LIFE while you have it.
Invisible Disabilities and the Workforce
CF, health, hearing loss, politics, essaysCommentFun medical equipment from the 1980s....
Take a look at the picture of me on the sidebar. (If you're reading this in email, click through.)
What do you see?
I'm not asking for an assessment of my physical attractiveness, or lack thereof. But if you just looked at that picture, you would think, yes. She looks like a pretty typical 30ish woman.
This is what you'd be missing:
*You can't see my cochlear implant, tucked behind my left ear. I don't wear any hearing devices in my right ear, and there's only about 20% natural hearing left there.
*The scar on my forehead? You can see that, but you probably don't know it's from a skin cancer removal. You also can't see the bald patch on the back of my head, from another one. Skin cancer is 10x more common in post-transplant people, because of our immunosuppression. It's not because I'm fair. (And I'm religious about sun protection, anyway).
*You can't see that I've got about 52% lung function--which for me is good. That's great! But for normal people, if it's lower than 70%, there's probably an issue. For me, 70% is a dream I will never see again, after hitting it in 1997. So imagine working without one lung. That's me all the time--and that's GREAT. I LOVE IT!
*You can't see the burn on my right arm, which is left over from transplant surgery. Third degree burn. Skin graft. It's rendered my right arm usable--thank God I still have it!--but it doesn't have complete function like it used to. (Knitting probably helps, though, in making it stronger.) The skin is very, very delicate. It tears easily. So I can't do a lot of manual labor with this arm--and this is my dominant arm. If you were looking at me, you'd notice, but you wouldn't have all that information.
*Oh, and I'm anemic. I always have been. Part of the paleness. :) But that affects my stamina, too. I'm used to it, now, but there are times when I need red meat and sleep--Moreso than the average bear.
I'm telling you all this because invisible disabilities have been in the news lately, as a part of the new Medicaid standards the administration is considering. I look pretty "able bodied", but I'm not--as any physical exam would show. I can't use a telephone--I use FaceTime, but not a real phone. If you call me, I can't understand you. You will sound like Charlie Brown's teacher. Being immunocompromised means if I get sick, there could be a hospital stay in my future. You get the flu, you stay home. I get the flu, I can end up in the hospital. I need to be more circumspect about where I go, especially during flu season. And honestly, I need to take care of my body. That means giving it enough sleep, among other things.
So, looking at me, you can't see these issues. But they're there. And when you compare me to an average 35 year old woman, it becomes apparent. Invisible disabilities are real. Ask anyone who has arthritis, for example. Or diabetes. Or epilepsy (which I had as a kid). They're not to be taken lightly. Just because someone looks able-bodied, doesn't mean she is able-bodied.
As a society, we need to be cognizant of that. I'm not making policy suggestions, here, but we need to be aware that there are serious disabilities that people cannot see, and that can impact ability to work. For example, I look fine. But you don't want me to be your receptionist, or ask me to carry heavy things or fix machinery on a regular (or even semi-regular) basis. And of course, I see many more doctors than average people. I see my transplant doctor every four months--I see my ENT every four months. I see my dermatologist very frequently, and I have days where I'm out having Mohs surgery, or having things removed--that takes time. I can have surgeries scheduled at the drop of a hat. Any employers who hires me needs to be aware of those things, and needs to be flexible about them. If they're not, then I'm in trouble. And my employer won't be happy, no matter how great my work is, or how intelligent I am. Without that understanding and flexibility, a job will be hard for both of us.
I want to provide this as food for thought, when you read about invisible disabilities, or work requirements. It's not wanting to work--it's things that make working difficult, for both employer and employee.
*
Having said that, though, I don't think a person with a disability or a chronic illness should automatically go the SSDI/Medicaid route. Here's why.
I think that being "normal", as much as you can, is good for self-image, self-esteem, and general mental health. I know that one of my biggest drivers growing up was that I was not going to be babied. I was going to be normal. That meant, doing my homework. Going to school. Taking exams. Etc. If I needed accommodation, I asked for it, but it was low-key. I finished high school. I went to college. And after college, I got a job.
I knew that I would need a job with good insurance. So yes, if you have medical issues, that means you have to consider jobs with good benefits. It doesn't mean you can go off and join a non-profit that doesn't provide good medical coverage, OK? You have to be reasonable and logical. I wrote more about this here.
I do not think it is a good idea for people with CF to sit around at home and bewail their state. First off, that would have driven me insane. Really. When I had to be home for four months post-transplant, after about month three, I was going stir-crazy. I have to have things to do.
But--there comes a time, when yes, you can't work anymore. This happened with my friend Sage. When she was listed for transplant, she had to leave her job and apply for SSDI. That does happen. It's part of life. But I don't think--and we talked about this often, so I know we agreed here--that she wouldn't wanted to sit at home, either.
Maybe you do. OK. But my feeling is, if you can contribute, contribute. BUT that requires having an employer that is flexible and that is willing to work with you. And I had that--until I didn't. Once that goes away, then life can get very difficult, and then it might be time for SSDI/Medicaid/whatever. If that time comes, then go for it. That's when people on the government side need to realize that we might look pretty able-bodied. But we're not.
And also, when it comes to the Medicaid/SSDI system, a lot of the time, they're not talking disability like I have a disability. They're talking about worker's comp sort of stuff. Like, back problems. Problems with limbs, or standing for eight hours, and movement. The system isn't really designed for people who have chronic issues that aren't movement/skeletally based. That is frustrating, because what I have is what I have. I'm never going to get my hearing back. My lung function may go a little higher, but this is pretty much as good as it gets. I'm never going to get better skin on my skin graft. So the government side of this needs to realize that some disabilities don't get better. They might stay stable--or they might radically get worse--but "better" is not going to happen.
I know that before I had to deal with all this, I had no idea that any of this was true. So I think it's worth it to share these thoughts with people, so you can realize that when government talks about "disability", there are levels, and there are degrees.
The Fiction of a Painless Life
CF7 CommentsMe with my best friend, Anne (on the right), after our First Communion Mass in April 1990. I had just turned eight years old. I wouldn't be diagnosed with CF until three years later.
I have almost died five times.
This is what it feels like.
It is very easy, for starters. All you'd have to do is...nothing. Just sleep more, let the energy and life flow away. It's silent, it's simple. It really is like falling asleep. It's so easy.
It's much harder to be alive, because in life, you have to fight for it.
I have almost died five times.
I almost lost my right arm.
I've lost most of my hearing.
I have almost no vein access, anywhere but via the port-a-cath that's surgically implanted in my chest.
I've learned to give myself insulin injections.
My parents and siblings know how to re-constitute IV meds.
I've had an IV line bleed out the night before my Algebra II final.
I've had skin cancer, epilepsy, cystic fibrosis, thalessimia minor, and a double lung transplant. I've had tuberculosis and an infection that only one other person in the world had had.
I've been to the ER so many times that it's like Cheers.
I've had pancreatitis eight times. If you haven't had it, be glad you haven't had it.
I've had four chest tubes.
I've taken pills every day of my life since I was two years old.
I could probably give myself chest X-rays by now.
I'm surprised I don't glow in the dark, due to all the radiation exposure I've had.
I've been twenty years old and planned my own funeral.
I've spent most holidays in the hospital except Christmas and my birthday.
I use the word "contraindicated" like most people use the word "like".
Every month, my mom pokes me with a needle and I don't hit her for it. :)
I have coughed up blood.
I have had 17% lung function.
I have been in a medically-induced coma for two weeks.
I've had people tell me that my CF treatments, which kept me alive, annoyed them. I've had people say injecting insulin is gross--to my face. I've had people ask rude questions, time and time again. I had a classmate tell me that there wasn't any point in me studying, because I was going to die.
But you know what?
I am still alive.
And I love my life, even with all its imperfection, even when it would've been easier to just let go and sail off into the West like Frodo.
But this life is exquisite, no matter what.
This world isn't my home. I know that. But it's so beautiful.
Because you know what's beautiful?
That I'm freaking typing this.
That I am breathing.
That I'm going to see my brother get married. That I've seen my godson grow up--because there was a time when I thought I wouldn't.
Standing in the Pacific Ocean.
Learning to knit.
Watching little kids smear Oreo crumbs on their faces.
Editing.
Writing.
Snuggling in bed.
Reading books.
Tickling babies.
Reading Robin Hood to enraptured small children and doing all the voices.
Christmas shopping.
Watching hockey games, and yelling at my team when they suck.
Learning to draw.
Eating a Duck Donut.
Eating anything, at all.
The couch I'm sitting on.
Godless on Netflix.
The Outlander series.
The Wizard of Oz.
Elizabeth Bennet.
Pretty dresses.
My sister's cat.
My siblings.
Fish and chips.
All of those things--all of those beautiful things--do not exist without the list of ugly things.
There is no life without suffering. There is no life without pain.
And yet, people try to limit it by killing people like me. By eliminating people with CF, or Down Syndrome, or by saying that assisted suicide, euthanasia, and abortion is the compassionate choice. That it's better to be dead than alive with a hard life. That it's better to not exist than to exist with pain.
I will never believe that. And I will never stop fighting for my right to exist, for my right to be here and to live the life that God has given me to live. And I will fight for all the other people like me, who are told that we shouldn't be here, that our lives are worthless because they are painful, because they make other people's lives hard, because we suffer.
Suffering has made me better. It has made me stronger. Without it, I would've been a pale imitation of myself.
My parents didn't kill me, obviously. My parents never went to court and said that my birth was "wrongful". They never made me feel like I was a drain on them, even though at times I've felt that way. They've always told me that I am worth it.
We are all worth it.
If you think that living with pain means life isn't worth living, then what are you doing here?
"Life is pain, princess," said Dread Pirate Roberts. He was right.
But there is also so much beauty in it.
The very chance to exist--to be brought into existence--the chance to have this life? This is everything.
And if you don't understand that, I pity you.
I am not brave
essays, health, transplant, CF2 CommentsLet's just get this out of the way.
I am not brave.
I am not courageous.
I am definitely not a saint.
Yet, people call me, and people like me, these things.
This makes me really uncomfortable.
Having CF, and having a transplant, do not make me brave.
Are you brave when you get up, get dressed, have your breakfast, and go to work? When you do the dishes and get the mail and pay the bills? No. You're living your life and being responsible.
When I did my treatments, took my enzymes, went to clinic, did IV meds...that was my life. When I take my meds in the morning, when I go to clinic now, that's my life. That's completely normal to me. It's not brave. It's not courageous.
Deciding to have a transplant? It was just deciding to live my life, to do what I needed to do to extend it. I wasn't afraid of dying on the table, because I knew without the surgery, I'd die anyway. So, choosing transplant wasn't brave. It was pragmatic.
Going to college? Getting my degree? Working? Again, no brave. Not courageous. Living my life. That's all.
When I see stories about how "Brave" people like me are, because we live with illness, I want to scream. It's not brave. It's just doing what you have to do with the hand you're dealt. What would you do? Curl up in a ball and refuse to leave your room? Refuse to do treatments? I guess. I knew CF people who did.
Bravery and courage are not what I have. I hated selling Girl Scout cookies. I'm not brave. I won't sky dive or even do a high-ropes course. I'm NOT A SAINT. I just am. I live my life the way all the rest of you do. This morning, I took my pills with my coffee. I've been taking pills with my breakfast since I was about two years old. It's not out of the ordinary. It's not brave. I'm not brave when I "let" people stick me multiple times to get an IV in. That's not bravery. That's what I have to do. What's my other option?
My parents are brave. They hold it together when everything is threatening to fly apart. I am not brave. I'm just doggedly stubborn.
Brave people are the people who rushed into the World Trade Centers on 9/11 to save the people inside, knowing they would probably die. Navy SEALs are brave people. Soldiers, firemen, nurses, first responders--they're brave. I don't put my life on the line. I don't do anything to save other people.
So please don't call me brave. I'm not.
********************************************
(Catholic 101 is now available! Pick up your copy here: https://gum.co/RMkqu)